Cholesterol is far more than just a number on your lab report—it’s a crucial waxy substance your liver produces to support essential bodily functions like hormone creation and cell membrane maintenance. However, when certain types of cholesterol accumulate in excess, particularly LDL or “bad” cholesterol, they can silently build up in your arteries and significantly increase your risk of heart disease and stroke. Understanding your cholesterol profile, knowing when and how to test it, and taking evidence-based steps to optimize your levels can be transformative for your long-term cardiovascular health.
This comprehensive guide will help you navigate the fundamentals of cholesterol testing and management, from interpreting your lipid panel results to understanding the latest 2025 guidelines that emphasize earlier screening and personalized treatment approaches. Whether you’re newly concerned about your numbers or looking to stay proactive about heart health, accessible testing options and lifestyle strategies can empower you to take control of your cholesterol levels and work effectively with your healthcare provider.

Cholesterol Fundamentals: Why Your Body Needs It
Your body relies on cholesterol for several critical biological processes that keep you healthy and functioning properly. This essential lipid serves as a building block for cell membranes throughout your body, ensuring they maintain proper structure and flexibility. Additionally, cholesterol is vital for producing steroid hormones like testosterone and estrogen, synthesizing vitamin D when your skin is exposed to sunlight, and creating bile acids that help digest dietary fats.
The challenge arises because your liver already produces all the cholesterol your body needs—typically about 1,000 milligrams daily. When you consume additional cholesterol through foods like eggs, meat, and dairy products, or when genetic factors cause overproduction, levels can climb beyond what’s healthy. The problem isn’t cholesterol itself, but rather having too much of the wrong type circulating in your bloodstream, particularly LDL cholesterol that can accumulate in artery walls.
What’s in a Lipid Panel?
A standard lipid panel measures four key components that together paint a picture of your cardiovascular risk. Total cholesterol represents the sum of all cholesterol types in your blood, while LDL cholesterol specifically measures the “bad” cholesterol particles most likely to cause arterial plaque buildup. HDL cholesterol, often called “good” cholesterol, helps transport cholesterol away from arteries back to the liver for processing. Finally, triglycerides measure blood fats that, when elevated, can contribute to heart disease risk.
Modern testing has evolved to be more convenient than ever. Non-fasting lipid panels are now widely accepted by medical professionals because they provide reliable results for total cholesterol, LDL, and HDL measurements without requiring you to skip meals. Only if your triglycerides are significantly elevated (above 400 mg/dL) might your healthcare provider request a fasting repeat test for more accurate triglyceride measurement.
HDL vs. LDL: Balancing “Good” and “Bad” Cholesterol
Understanding the fundamental difference between HDL and LDL cholesterol is crucial for making sense of your test results and cardiovascular risk. LDL particles transport cholesterol from your liver to tissues throughout your body, but when present in excess, they can penetrate artery walls and trigger inflammation that leads to plaque formation. This process, called atherosclerosis, narrows arteries and restricts blood flow to vital organs like your heart and brain.
HDL cholesterol works in the opposite direction, picking up excess cholesterol from tissues and arterial walls and transporting it back to the liver for recycling or elimination. While this “reverse cholesterol transport” is generally protective, recent research has shifted focus toward reducing the total burden of atherogenic particles (primarily LDL) rather than simply trying to raise HDL levels. Some people naturally have low HDL but maintain excellent cardiovascular health when their LDL and overall inflammatory markers remain optimal.
Evidence-Based Targets
Current guidelines establish clear targets for optimal cholesterol levels, though individual goals may vary based on your overall cardiovascular risk profile. Total cholesterol should ideally remain below 200 mg/dL, with LDL cholesterol under 100 mg/dL for most people. However, individuals with diabetes, established heart disease, or multiple risk factors may benefit from even lower LDL targets of 70 mg/dL or less.
For HDL cholesterol, men should aim for levels above 40 mg/dL while women should target above 50 mg/dL. Triglycerides are considered optimal when they remain below 150 mg/dL. Non-HDL cholesterol, calculated by subtracting HDL from total cholesterol, provides another useful marker—it should typically stay below 130 mg/dL for most people, representing the total burden of potentially harmful cholesterol particles.

Understanding Your Numbers: What Results Really Mean
Interpreting your lipid panel results involves more than simply comparing numbers to standard ranges—it requires understanding how different components work together to influence your cardiovascular risk. Your lipid profile provides a snapshot of cholesterol metabolism and transport, but factors like family history, other health conditions, and lifestyle habits all influence how these numbers translate to actual heart disease risk.
Beyond the basic lipid panel, additional markers can provide valuable insights for certain individuals. Apolipoprotein B (ApoB) measures the actual number of atherogenic particles in your blood, which can be more informative than LDL levels alone, especially for people with diabetes or metabolic syndrome. Lipoprotein(a), or Lp(a), represents a genetic risk factor that affects approximately 20% of the population and can significantly increase heart disease risk even when other cholesterol levels appear normal.
When considering how often to recheck your cholesterol, general recommendations suggest testing every 4-6 years starting at age 20 for people without risk factors. However, if you have diabetes, family history of heart disease, or other risk factors, more frequent monitoring every 1-2 years may be appropriate. The timing also depends on whether you’re actively treating elevated levels—lifestyle changes or medications typically warrant retesting within 6-12 weeks to assess response.
The significance of cholesterol management becomes clear when considering that approximately 54.5% of US adults have blood cholesterol levels above recommended ranges, contributing to cardiovascular disease remaining the leading cause of death worldwide. This widespread prevalence emphasizes why regular screening and proactive management are essential components of preventive healthcare.
Genetics and Family History: When Cholesterol Runs in Families
Family history plays a profound role in cholesterol levels and cardiovascular risk, with some individuals inheriting genetic variations that dramatically affect how their bodies produce, process, or eliminate cholesterol. The most significant of these conditions is familial hypercholesterolemia (FH), a genetic disorder that affects approximately one in 250 people worldwide and causes severely elevated LDL cholesterol levels from birth.
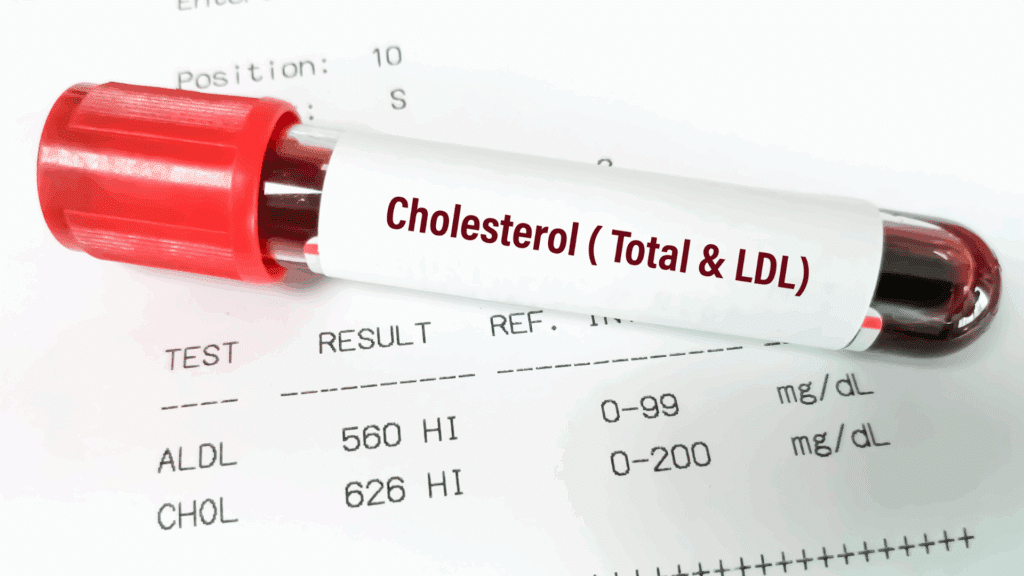
People with FH typically have LDL cholesterol levels of 190 mg/dL or higher, often reaching 300-500 mg/dL or more without treatment. This genetic condition occurs when individuals inherit defective genes that impair the body’s ability to remove LDL cholesterol from the bloodstream. Those who inherit one defective gene copy (heterozygous FH) have significantly elevated cholesterol, while the rare individuals who inherit defective genes from both parents (homozygous FH) can have extraordinarily high levels requiring aggressive treatment from childhood.
Recognizing and Managing Genetic Risk
The consequences of undiagnosed and untreated FH can be severe. Men with FH face up to a 50% risk of heart attack by age 50, while women have up to a 30% risk by age 60—decades earlier than the general population. This dramatically accelerated timeline makes early identification and treatment crucial for preventing premature cardiovascular events.
If you have a family history of early heart disease (men under 55, women under 65), very high cholesterol levels, or physical signs like tendon xanthomas (cholesterol deposits), consider discussing FH screening with your healthcare provider. Genetic testing and cascade screening of family members can identify affected relatives who might benefit from early intervention. Treatment for FH typically requires more intensive approaches, including high-dose statins, additional medications like PCSK9 inhibitors, and sometimes specialized procedures like LDL apheresis.
How Age and Sex Influence Cholesterol
Cholesterol levels naturally change throughout life due to hormonal fluctuations, metabolic changes, and the cumulative effects of lifestyle factors. Understanding these patterns can help you set appropriate expectations and work with your healthcare provider to establish personalized targets that account for your life stage and risk profile.
Men typically develop elevated cholesterol and cardiovascular risk at younger ages compared to women, with LDL levels often rising during their 30s and 40s. This earlier onset helps explain why men face heart disease risk approximately 10 years sooner than women. However, the protective effects of estrogen in premenopausal women don’t last forever—after menopause, women’s cholesterol levels often rise significantly, and their cardiovascular risk accelerates to eventually match or exceed that of men.
Age-related changes in cholesterol metabolism occur for several reasons. Liver function may become less efficient at regulating cholesterol production and clearance. Physical activity often decreases with age, affecting how the body processes fats and sugars. Additionally, other health conditions that commonly develop with aging—such as diabetes, thyroid disorders, or kidney disease—can further influence cholesterol levels and require more intensive management strategies.
Subtle Signs to Watch: When You Might Not “Feel” High Cholesterol
One of the most challenging aspects of managing cholesterol is that elevated levels rarely cause noticeable symptoms until serious complications develop. Unlike high blood pressure, which might cause headaches, or diabetes, which can cause increased thirst and urination, high cholesterol typically remains completely silent for years or even decades while gradually damaging your arteries.
The absence of symptoms doesn’t mean high cholesterol is harmless—quite the opposite. This silent nature allows cholesterol-driven atherosclerosis to progress undetected, with the first “symptom” sometimes being a heart attack or stroke. By the time chest pain, shortness of breath, or other cardiovascular symptoms appear, significant arterial damage has likely already occurred.
In rare cases, extremely high cholesterol levels might produce visible signs. These can include xanthomas—yellowish cholesterol deposits that appear as bumps on tendons, elbows, knees, or around the eyes—or a gray or white arc around the cornea of the eye called arcus senilis. However, these physical signs typically only occur with severe genetic conditions like familial hypercholesterolemia or after decades of very poor cholesterol control.
The key takeaway is that regular screening, not waiting for symptoms, remains your best defense against cholesterol-related complications. This proactive approach allows you to identify and address problems while they’re still manageable through lifestyle changes or medications, rather than waiting until irreversible damage has occurred.
Testing Made Easy: Fasting vs Non-Fasting, What to Order
Modern cholesterol testing has become significantly more convenient and accessible, with important changes in testing protocols that make it easier than ever to monitor your levels regularly. The most significant advancement is the widespread acceptance of non-fasting lipid panels, which eliminate the need to skip meals before testing while still providing accurate and clinically useful results.
Non-fasting lipid testing provides reliable measurements for total cholesterol, LDL cholesterol, and HDL cholesterol, with minimal differences compared to fasting results. The only component that shows significant variation based on recent food intake is triglycerides, which can rise temporarily after meals. However, even non-fasting triglyceride levels provide valuable information—if they’re elevated above 175 mg/dL on a non-fasting test, your healthcare provider might recommend a fasting repeat to get a more precise measurement.
Beyond the Basic Panel
While a standard lipid panel provides essential information for most people, additional tests can offer deeper insights into cardiovascular risk, particularly for individuals with family history, diabetes, or other risk factors. Apolipoprotein B (ApoB) measures the actual number of atherogenic particles in your blood, which can be more informative than LDL levels alone, especially in people with diabetes, metabolic syndrome, or discordant HDL/triglyceride ratios.
Lipoprotein(a), commonly abbreviated as Lp(a), represents an important genetic risk factor that standard cholesterol testing doesn’t capture. Elevated Lp(a) affects approximately 20% of the population and can significantly increase cardiovascular risk even when other cholesterol levels appear optimal. Testing Lp(a) once in your lifetime can help identify this inherited risk factor and guide more aggressive treatment strategies when necessary.
Treatment and Optimization: Lifestyle, Medications, and What’s New
Effective cholesterol management typically begins with evidence-based lifestyle modifications that can significantly improve your lipid profile while providing numerous other health benefits. The foundation of cholesterol optimization rests on dietary approaches that emphasize whole foods, regular physical activity, weight management, and elimination of smoking—strategies that work synergistically to improve not just cholesterol levels but overall cardiovascular health.
Mediterranean-style eating patterns consistently demonstrate powerful effects on cholesterol levels and heart disease prevention. This approach emphasizes olive oil, nuts, seeds, fatty fish, vegetables, fruits, whole grains, and legumes while limiting red meat, processed foods, and refined sugars. Specific dietary components like soluble fiber from oats, beans, and apples can directly lower LDL cholesterol by 5-10%, while plant sterols and stanols found in fortified foods or supplements can provide additional reductions.
Regular aerobic exercise, even moderate activities like brisk walking for 150 minutes per week, can raise HDL cholesterol by 5-15% while improving insulin sensitivity and helping with weight management. Resistance training provides complementary benefits, particularly for improving body composition and metabolic health.
Medication Options and Guidelines
When lifestyle changes alone aren’t sufficient to achieve target cholesterol levels, medications provide proven options for reducing cardiovascular risk. Statins remain the first-line treatment for most people, with extensive research demonstrating their ability to lower LDL cholesterol by 30-50% while reducing heart attack and stroke risk by approximately 25-35%.
For individuals who cannot tolerate statins or need additional LDL reduction, several newer options are available. Ezetimibe blocks cholesterol absorption in the intestines and can lower LDL by an additional 15-20%. Bempedoic acid, a newer oral medication, provides statin-like effects through a different mechanism and may be better tolerated by people with statin-related muscle problems. PCSK9 inhibitors, available as injectable medications or newer oral formulations, can dramatically lower LDL cholesterol by 50-60% and are particularly valuable for people with familial hypercholesterolemia or very high cardiovascular risk.
2025 Guidelines and Emerging Approaches
The latest cholesterol management guidelines reflect important shifts in screening and treatment philosophies. The 2025 European guidelines emphasize systematic evaluation beginning at age 40, recognizing that earlier intervention can prevent more cardiovascular events than waiting until problems develop. This approach acknowledges that atherosclerosis begins decades before symptoms appear, making earlier identification and treatment crucial for optimal outcomes.
Personalized medicine approaches are becoming increasingly sophisticated. Machine learning tools are being developed to predict individual responses to specific treatments, potentially allowing healthcare providers to optimize therapy choices and dosing more precisely. These technologies may help identify which patients are most likely to achieve target LDL levels with specific medications, reducing trial-and-error approaches and improving treatment efficiency.
The growing attention to Lipoprotein(a) levels represents another important evolution in cardiovascular risk assessment. While treatments specifically targeting Lp(a) are still in development, identifying elevated levels can guide more aggressive management of other risk factors and potentially earlier consideration of advanced therapies.
FAQs
What is cholesterol and why is it important?
Cholesterol is a waxy, fat-like substance that your liver produces naturally and that you also obtain from certain foods. Your body needs cholesterol to build cell membranes, produce hormones like testosterone and estrogen, synthesize vitamin D, and create bile acids for fat digestion. However, when you have too much cholesterol, particularly LDL or “bad” cholesterol, it can build up in your artery walls and increase your risk of heart disease and stroke.
What’s the difference between LDL and HDL cholesterol?
LDL (low-density lipoprotein) cholesterol carries cholesterol from your liver to tissues throughout your body, but excess LDL can deposit cholesterol in artery walls, leading to plaque buildup and increased cardiovascular risk. HDL (high-density lipoprotein) cholesterol works in reverse, picking up excess cholesterol from tissues and arterial walls and transporting it back to your liver for processing or elimination, which is why it’s often called “good” cholesterol.
What are healthy cholesterol numbers?
For optimal cardiovascular health, total cholesterol should be below 200 mg/dL, LDL cholesterol should be under 100 mg/dL (or lower for high-risk individuals), HDL cholesterol should be above 40 mg/dL in men and 50 mg/dL in women, and triglycerides should remain below 150 mg/dL. However, your individual targets may vary based on your overall cardiovascular risk profile, family history, and other health conditions.
How does family history affect cholesterol risk?
Family history significantly influences cholesterol levels and cardiovascular risk through genetic factors. The most dramatic example is familial hypercholesterolemia (FH), which affects about 1 in 250 people and causes severely elevated LDL cholesterol from birth due to inherited genetic defects. People with FH face dramatically increased heart disease risk, with men having up to 50% risk of heart attack by age 50 and women having up to 30% risk by age 60, making early identification and aggressive treatment crucial.
When should I have my cholesterol tested?
General guidelines recommend cholesterol screening every 4-6 years starting at age 20 for people without risk factors. However, the 2025 guidelines emphasize more systematic evaluation beginning at age 40, recognizing that earlier intervention can prevent more cardiovascular events. If you have diabetes, family history of heart disease, or other risk factors, more frequent testing every 1-2 years may be appropriate, and you might benefit from additional markers like ApoB or Lipoprotein(a).
Conclusion
Understanding and managing your cholesterol levels represents one of the most impactful steps you can take for long-term cardiovascular health. By grasping the fundamentals of how different types of cholesterol affect your body, knowing your target numbers, and implementing evidence-based lifestyle strategies, you can significantly reduce your risk of heart disease and stroke while improving your overall well-being.
The evolution of cholesterol testing and treatment offers more options and convenience than ever before. Non-fasting lipid panels make regular monitoring easier, while advances in personalized medicine and new treatment options provide hope for even the most challenging cases. Whether you’re just beginning to pay attention to your cholesterol levels or looking to optimize an existing management plan, the key is taking action based on current evidence and working collaboratively with your healthcare provider.
Take the next step in your cholesterol management journey by ordering a comprehensive lipid panel to establish your baseline numbers. Consider adding advanced markers like ApoB or Lipoprotein(a) if you have family history or other risk factors. Use these results to set specific goals with your healthcare provider, implement targeted lifestyle changes, and schedule follow-up testing in 8-12 weeks to track your progress. Your future self will thank you for taking proactive steps today to protect your cardiovascular health.
Explore Related Topics
Dive deeper into specific aspects of cholesterol management with these comprehensive resources designed to expand your understanding and support your health journey:
What Is Cholesterol and Why Does Your Body Need It? – Discover the essential biological functions of cholesterol and learn why this vital substance becomes problematic only when present in excess or the wrong proportions.
HDL vs LDL Cholesterol: Understanding Good vs Bad Cholesterol – Explore the crucial differences between protective and harmful cholesterol types, including how they function in your body and why the balance between them matters for heart health.
Cholesterol Numbers Explained: What Your Test Results Really Mean – Learn to interpret your lipid panel results with confidence, understand optimal ranges for different age groups, and know when your numbers warrant concern or celebration.
Family History and Cholesterol: Understanding Genetic Risk Factors – Uncover how inherited genetic variations influence your cholesterol levels and cardiovascular risk, with special focus on conditions like familial hypercholesterolemia that require specialized management approaches.
Age, Gender, and Cholesterol: How Demographics Affect Your Levels – Understand how cholesterol naturally changes throughout different life stages and why men and women face varying patterns of cardiovascular risk as they age.
Early Warning Signs of High Cholesterol You Shouldn’t Ignore – Learn to recognize subtle indicators and risk factors that might signal elevated cholesterol levels, even though this condition typically remains silent until complications develop.





