Introduction
Environmental toxins represent an often overlooked threat to liver health, with daily exposure occurring through the air we breathe, water we drink, food we consume, and products we use. The liver serves as the body’s primary detoxification center, processing and neutralizing thousands of chemical compounds that enter our system each day. This critical role makes the organ particularly vulnerable to damage from environmental contaminants, which can accumulate over time and overwhelm the liver’s natural protective mechanisms.
Daily exposure to common pollutants has cumulative effects on liver health, even at levels previously considered safe. Modern life exposes individuals to an unprecedented array of synthetic chemicals, air pollutants, and industrial byproducts that can trigger inflammation, disrupt metabolism, and contribute to chronic liver disease. Understanding these exposures and their health implications empowers individuals to make informed decisions about protection and monitoring strategies.
Common Environmental Toxins Affecting Liver Health
Environmental toxins that impact liver health span a diverse range of compounds encountered in everyday life, from air pollutants to synthetic chemicals in household products. These substances can affect liver function through various mechanisms, often working synergistically to create greater damage than individual exposures might suggest. Recognizing the most significant toxin sources helps prioritize protective measures and guide testing decisions.
Air Pollution (PM2.5)
Fine particulate matter, known as PM2.5 due to its diameter of 2.5 micrometers or smaller, represents one of the most pervasive environmental threats to liver health. Recent studies show long-term PM2.5 exposure correlates with advanced liver complications, including non-alcoholic fatty liver disease, liver fibrosis, and increased cancer risk. These microscopic particles can penetrate deep into the respiratory system and enter the bloodstream, where they trigger systemic inflammation that affects liver function.
Urban areas with heavy traffic, industrial zones, and regions affected by wildfire smoke show the highest PM2.5 concentrations. The liver’s role in filtering blood means it receives concentrated exposure to these particles, leading to oxidative stress and inflammatory responses. Long-term exposure has been linked to metabolic dysfunction, insulin resistance, and progression of fatty liver disease, even in individuals without traditional risk factors.
PFAS (“Forever Chemicals”)
Per- and polyfluoroalkyl substances, commonly known as PFAS or “forever chemicals,” accumulate in liver tissue due to their persistence in the environment and human body. Virtually all U.S. adults have detectable PFAS levels, with elevated concentrations directly associated with liver damage markers and increased risk of non-alcoholic fatty liver disease. These synthetic compounds are found in water-resistant clothing, non-stick cookware, food packaging, firefighting foam, and countless household products.
PFAS chemicals resist natural breakdown processes, allowing them to bioaccumulate in liver tissue over decades. Once absorbed, these compounds can interfere with normal liver metabolism, disrupt lipid processing, and promote inflammation. The liver’s inability to effectively process and eliminate PFAS means that even low-level chronic exposure can lead to significant tissue concentrations and associated health effects.
Microplastics
Emerging research investigates microplastics’ possible role in liver inflammation and chronic disease, with these tiny particles now detected in human blood, organs, and tissues. Microplastics enter the body through ingestion of contaminated food and water, inhalation of airborne particles, and potentially through skin contact. The liver encounters these particles as they circulate through the bloodstream, where they may trigger immune responses and inflammatory processes.
Plastic particles can carry absorbed chemicals from their environment, acting as vehicles for delivering additional toxins directly to liver tissue. The long-term health consequences of microplastic accumulation remain under investigation, but early studies suggest potential links to metabolic disruption, oxidative stress, and cellular damage. The ubiquity of plastic in modern life means exposure is virtually unavoidable, making understanding and mitigation strategies increasingly important.
Pesticides & Food Contaminants
Agricultural pesticides, herbicides, and food processing chemicals contribute to liver toxicity through multiple pathways, including direct consumption of contaminated produce and environmental exposure from agricultural runoff. These compounds contribute to oxidative stress and metabolic disruption, with some pesticides specifically targeting cellular processes that are also critical for normal liver function.
Organophosphates, organochlorines, and glyphosate-based herbicides represent some of the most concerning pesticide classes for liver health. These chemicals can accumulate in fatty tissues, including the liver, where they may remain active for extended periods. Chronic exposure has been linked to increased rates of liver cancer, fatty liver disease, and liver enzyme abnormalities, particularly in agricultural workers and communities near farming operations.
Heavy Metals & Solvents
Occupational exposures to solvents, heavy metals, and industrial chemicals contribute to clusters of toxicant-associated liver disease, highlighting ongoing public health concerns in industrial and manufacturing settings. Lead, mercury, cadmium, and arsenic can accumulate in liver tissue, where they interfere with enzymatic processes and promote cellular damage. Organic solvents used in manufacturing, cleaning, and chemical processing can cause acute liver injury and contribute to chronic disease development.
Workers in industries such as metal processing, chemical manufacturing, electronics assembly, and automotive repair face elevated risks from these exposures. However, environmental contamination can affect broader populations through contaminated water supplies, air pollution, and consumer products containing heavy metals or solvent residues.
How Environmental Toxins Affect the Liver
Environmental toxins damage liver tissue through several interconnected mechanisms that can ultimately lead to chronic disease and organ dysfunction. Understanding these pathways helps explain why seemingly low-level exposures can have significant health consequences over time. The liver’s central role in detoxification means it experiences concentrated exposure to toxins, making it particularly vulnerable to cumulative damage from multiple environmental sources.
Mechanisms of toxin-induced liver damage include oxidative stress, chronic inflammation, altered metabolism, and DNA damage, all of which can occur simultaneously and reinforce each other’s effects. Oxidative stress results when toxin exposure overwhelms the liver’s antioxidant defenses, leading to cellular damage and dysfunction. Chronic inflammation develops as the immune system responds to persistent toxin presence, creating a cycle of tissue damage and attempted repair.
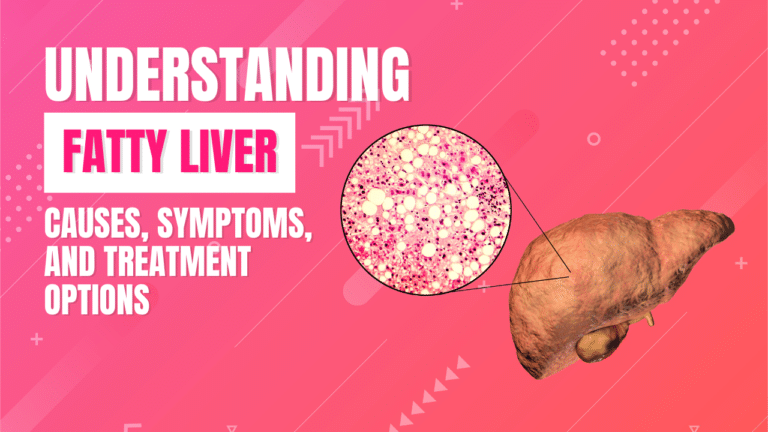
The progression from toxin exposure to clinical liver disease follows predictable patterns, with health outcomes including fatty liver disease (NAFLD/NASH), fibrosis, cirrhosis, and hepatocellular carcinoma representing increasingly severe stages of damage. Early changes may include enzyme elevation and fat accumulation, which can progress to inflammation and scarring if exposures continue. Advanced disease develops when the liver’s regenerative capacity is overwhelmed by ongoing damage.
Exposomics research is unveiling hidden contributors to liver disease by analyzing comprehensive environmental exposure patterns rather than focusing on individual toxins. This approach recognizes that people are exposed to complex mixtures of chemicals that may interact in unexpected ways, potentially amplifying risks beyond what individual compound studies might suggest.
High-Risk Groups & Vulnerabilities
Certain populations face elevated risks from environmental toxin exposure due to occupational factors, geographic location, age, or underlying health conditions. Understanding these vulnerability patterns helps identify individuals who may benefit from enhanced protective measures and more frequent monitoring. Risk assessment should consider both exposure intensity and individual susceptibility factors that may amplify toxin effects.
Individuals living in industrial or urban areas experience higher baseline exposures to air pollution, traffic-related toxins, and industrial chemicals. Proximity to manufacturing facilities, waste sites, or heavy transportation corridors can significantly increase exposure levels compared to rural or suburban environments. Environmental justice concerns arise when disadvantaged communities face disproportionate exposure burdens due to industrial siting decisions and limited resources for exposure mitigation.
Workers in industries involving chemical exposure face occupational risks that can far exceed environmental background levels. Manufacturing, agriculture, mining, construction, and chemical processing industries present particular concerns for solvent, metal, and pesticide exposures. Healthcare workers, firefighters, and laboratory personnel also face unique occupational exposure risks that require specialized protective measures.
People with pre-existing metabolic conditions such as diabetes, obesity, or fatty liver disease may be more susceptible to toxin-induced liver damage. These conditions can impair the liver’s detoxification capacity and regenerative ability, making individuals more vulnerable to environmental insults. Age-related changes in liver function mean that children and elderly individuals may have reduced capacity to process and eliminate environmental toxins effectively.
Prevention & Practical Strategies
Reducing environmental toxin exposure requires a comprehensive approach that addresses multiple sources and pathways while recognizing that complete avoidance is often impossible in modern life. Practical strategies focus on minimizing the most significant exposures while supporting the liver’s natural detoxification capacity through lifestyle measures. Regular monitoring helps track progress and identify potential problems before they become serious health concerns.
Lifestyle Adjustments
Simple dietary and household changes can significantly reduce toxin exposure without major lifestyle disruptions. Choosing organic produce, using glass or stainless steel containers instead of plastic, and avoiding processed foods help minimize pesticide and chemical exposure from food sources. Washing fruits and vegetables thoroughly, even organic varieties, removes surface residues and reduces ingestion of contaminated particles.
Water quality improvements through certified filtration systems can remove heavy metals, chemicals, and other contaminants that may stress liver detoxification systems. Point-of-use filters for drinking water and shower filters for bathing water help reduce overall exposure burden. Avoiding plastic water bottles, particularly those exposed to heat or sunlight, reduces microplastic and chemical leaching risks.
Personal care and household product choices significantly impact daily chemical exposure. Selecting products with fewer synthetic ingredients, avoiding artificial fragrances, and choosing cleaning products with simpler formulations reduces the chemical burden on liver detoxification systems. Reading ingredient labels and researching product safety through databases like the Environmental Working Group’s resources helps make informed choices.
Environmental Modifications
Home environment improvements can substantially reduce indoor air pollution and chemical exposures that affect liver health. HEPA air filtration systems remove particulate matter, allergens, and some chemical vapors from indoor air, creating a cleaner environment for daily living. Regular HVAC maintenance, including filter changes and duct cleaning, helps maintain optimal indoor air quality.
Proper ventilation during activities that generate chemical vapors, such as cooking, cleaning, or home improvement projects, prevents accumulation of potentially harmful compounds. Opening windows when outdoor air quality permits, using exhaust fans, and avoiding activities that generate fumes during poor outdoor air quality days helps minimize exposure risks.
Safe storage and disposal of household chemicals, paints, solvents, and other potentially toxic materials prevents accidental exposure and environmental contamination. Following manufacturer guidelines for use and storage, maintaining adequate ventilation during use, and participating in community hazardous waste disposal programs helps protect both individual and community health.
Healthcare & Testing
Regular liver function testing provides early detection of toxin-related damage before symptoms develop, enabling timely interventions that can prevent disease progression. Walk-In Lab’s comprehensive liver panels, including ALT, AST, GGT, and other markers, offer convenient access to essential monitoring tools without requiring physician referrals or insurance authorization. These tests can track liver health over time and identify changes that may indicate environmental toxin effects.
Specialized testing for heavy metals, organic chemicals, or specific toxin exposures may be appropriate for individuals with known high-risk exposures or unexplained liver abnormalities. Biomonitoring tests can identify current toxin levels in blood or urine, providing objective data about exposure intensity and helping guide protective interventions.
Working with healthcare providers familiar with environmental health issues ensures appropriate interpretation of test results and development of comprehensive management strategies. Environmental medicine specialists can provide expertise in toxin exposure assessment, testing interpretation, and evidence-based intervention strategies tailored to individual risk profiles.
Frequently Asked Questions
What toxins are most harmful to the liver?
Air pollution (particularly PM2.5), PFAS chemicals, pesticides, microplastics, and heavy metals represent the most significant environmental threats to liver health based on current research. These toxins are particularly concerning because they are widespread in the environment, can accumulate in liver tissue, and have been directly linked to liver inflammation, fatty liver disease, and increased cancer risk in multiple studies.
Can liver damage from toxins be reversed?
Early-stage liver damage, including fatty infiltration and mild inflammation, can often improve with lifestyle changes and removal of toxin exposures. However, advanced fibrosis and cirrhosis are typically irreversible, making early detection and intervention crucial. The liver’s remarkable regenerative capacity means that significant improvement is possible if toxin exposure is reduced before permanent structural damage occurs.
How do I know if toxins are affecting my liver?
Blood tests measuring liver enzymes (ALT, AST, GGT) and other liver function markers can detect early signs of toxin-related damage before symptoms appear. Advanced imaging studies like FibroScan can assess liver stiffness and fat content, providing additional information about toxin effects. Regular testing is particularly important for individuals with known high-risk exposures or unexplained symptoms like fatigue, abdominal pain, or digestive issues.
How can I reduce my exposure to environmental toxins?
Practical steps include filtering drinking water, limiting plastic use (especially for food storage), choosing organic produce when possible, using air purifiers with HEPA filters, selecting safer personal care and cleaning products, and avoiding areas with heavy air pollution when feasible. Complete elimination isn’t possible, but these measures can significantly reduce overall toxin burden and support liver health.
Who is most at risk for toxin-related liver damage?
Industrial workers, urban residents with high air pollution exposure, people with occupational chemical exposures, individuals with pre-existing liver or metabolic conditions, and those living near contaminated sites face elevated risks. Children and elderly individuals may also be more susceptible due to differences in toxin processing capacity. Geographic factors, lifestyle choices, and genetic variations in detoxification capacity can all influence individual risk levels.
Conclusion
Environmental toxins represent a significant but manageable threat to liver health, with daily exposures from air pollution, synthetic chemicals, and industrial compounds contributing to the rising burden of liver disease worldwide. While complete avoidance of environmental toxins is impossible in modern life, understanding exposure sources and implementing targeted protective strategies can substantially reduce risks and support optimal liver function.
The liver’s central role in detoxification makes it particularly vulnerable to environmental insults, yet its remarkable capacity for regeneration means that early interventions can prevent or reverse many forms of toxin-related damage. Simple lifestyle modifications, environmental improvements, and regular health monitoring create a comprehensive approach to liver protection that addresses both current exposures and long-term health preservation.
Proactive testing through accessible services like Walk-In Lab enables early detection of liver changes before symptoms develop, providing opportunities for timely intervention when they can be most effective. Regular liver function panels, combined with awareness of environmental risks and implementation of protective strategies, offer a practical pathway to maintaining liver health despite unavoidable environmental exposures. Order a liver function test with Walk-In Lab today to detect and manage potential toxin-related risks early, taking a crucial step toward protecting your long-term liver health.
This article is for informational purposes only and not a substitute for medical advice. Always consult your healthcare provider for guidance regarding your specific health concerns and environmental exposure risks.