The liver stands as one of the most remarkable organs in the human body, serving as both a master detoxifier and metabolic powerhouse. Every minute of every day, this vital organ performs hundreds of essential functions that keep you alive and healthy. From processing the food you eat to neutralizing harmful substances, the liver works tirelessly behind the scenes to maintain your body’s delicate biochemical balance.
Understanding how your liver works empowers you to make informed decisions about your health and recognize the importance of preventive care. This comprehensive guide explores the liver’s critical functions, from detoxification and metabolism to immunity and regeneration, while highlighting why regular monitoring through simple lab tests can help you maintain optimal liver health throughout your life.
The Liver’s Role in Detoxification
The liver serves as your body’s primary detoxification center, processing and neutralizing countless harmful substances that enter your system daily. This complex process involves sophisticated enzyme systems that transform potentially dangerous compounds into harmless, water-soluble substances that can be safely eliminated from your body.
How Detox Works
The liver’s detoxification process operates through two main phases, primarily driven by a family of enzymes called cytochrome P450. These enzymes work like molecular scissors, chemically modifying toxins to make them easier to process. In Phase I, these enzymes break down substances through oxidation, reduction, or hydrolysis reactions. Phase II involves conjugation reactions, where the liver attaches water-soluble molecules to the modified toxins, making them ready for elimination through bile or urine.
This two-phase system is so efficient that it can process thousands of different compounds, from prescription medications to environmental pollutants. The liver’s ability to adapt its enzyme production based on exposure levels explains why some medications become less effective over time and why certain individuals may have different responses to drugs or alcohol.
Everyday Detox Examples
Your liver demonstrates its detoxification prowess through common, everyday scenarios. When you consume alcohol, specialized enzymes convert ethanol into acetaldehyde, then into harmless acetate that your body can easily eliminate. Similarly, when you take over-the-counter pain relievers like acetaminophen, liver enzymes process these medications to prevent toxic buildup while allowing the therapeutic effects to occur.
Environmental toxins from air pollution, cleaning products, and even natural plant compounds undergo this same detoxification process. The liver also processes metabolic waste products generated by your own cells, including ammonia from protein breakdown, which it converts into less toxic urea. Regular monitoring of liver enzymes like ALT and AST through comprehensive lab testing can provide valuable insights into how well your detoxification systems are functioning.
Metabolism: Fueling the Body
Beyond detoxification, the liver serves as your body’s metabolic command center, carefully regulating the processing and storage of nutrients from your diet. This organ acts like a sophisticated fuel management system, ensuring your cells receive the right nutrients at the right time while maintaining stable blood chemistry.
Carbohydrates
The liver plays a crucial role in blood sugar regulation through its management of carbohydrate metabolism. After you eat, the liver absorbs excess glucose from your bloodstream and converts it into glycogen, a storage form of sugar that can be rapidly mobilized when needed. During fasting periods or between meals, the liver breaks down stored glycogen back into glucose, releasing it into your bloodstream to maintain steady energy levels for your brain and other vital organs.
This glucose buffering system is so precise that healthy individuals maintain blood sugar levels within a narrow range despite varying food intake and physical activity. When glycogen stores become depleted during extended fasting or intense exercise, the liver can even manufacture new glucose from amino acids and other non-carbohydrate sources through a process called gluconeogenesis.
Fats
Liver fat metabolism involves both the breakdown of fats for energy and the synthesis of important lipid compounds. When you consume dietary fats, the liver helps process them into usable forms, breaking down fatty acids through beta-oxidation to produce energy. During periods of carbohydrate restriction or extended fasting, the liver can convert fats into ketones, which serve as an alternative fuel source for your brain and other organs.
The liver also synthesizes cholesterol, despite its negative reputation, which serves as a building block for hormones, cell membranes, and bile acids. Additionally, the liver produces lipoproteins that transport fats throughout your bloodstream, carefully packaging cholesterol and triglycerides for delivery to tissues that need them while removing excess fats from circulation.
Proteins
Protein metabolism in the liver involves the modification and processing of amino acids from dietary protein and the conversion of toxic ammonia into safer compounds. When proteins are broken down throughout your body, they release ammonia, a highly toxic substance that can damage cells, particularly in the brain. The liver efficiently converts this ammonia into urea through the urea cycle, allowing safe elimination through the kidneys.
The liver also modifies amino acids to create new proteins needed throughout your body and can convert amino acids into glucose when carbohydrate stores run low. This protein processing capability explains why individuals with severe liver disease often experience problems with protein metabolism and may develop complications related to ammonia buildup.
Bile Production and Digestion
The liver’s production of bile represents one of its most visible and important digestive functions. This greenish-yellow fluid serves dual purposes: aiding in fat digestion and serving as a vehicle for eliminating waste products from your body.
Your liver produces approximately 800 to 1,000 milliliters of bile daily, a remarkable volume that demonstrates the organ’s continuous metabolic activity. Bile contains bile salts, cholesterol, phospholipids, and bilirubin, each serving specific functions in digestion and waste elimination. The bile salts act like biological detergents, breaking down large fat molecules into smaller droplets that digestive enzymes can more easily process.
Bile also serves as the liver’s primary method for eliminating certain waste products, particularly bilirubin, which results from the breakdown of old red blood cells. When bile flow becomes impaired, bilirubin can accumulate in the blood and tissues, causing the yellowish discoloration known as jaundice. This connection between bile production and waste elimination highlights the liver’s integrated approach to maintaining body chemistry.
The relationship between liver health and digestive function extends beyond simple bile production. Recent research has revealed the importance of the gut-liver axis, showing how the health of your intestinal microbiome directly influences liver function and inflammation levels. This bidirectional communication system explains why digestive health and liver health are so closely interconnected.
Protein Synthesis: Building Blocks of Health
The liver serves as your body’s primary protein manufacturing facility, producing numerous essential proteins that circulate throughout your bloodstream and support vital physiological functions. This synthetic capability makes the liver unique among organs, as it creates proteins that your body cannot obtain from diet alone.
Albumin represents the liver’s most abundant protein product, accounting for about 60% of total blood proteins. This crucial protein maintains proper blood volume and pressure by creating osmotic pressure that keeps fluid within blood vessels rather than leaking into surrounding tissues. When albumin levels drop due to liver dysfunction, fluid can accumulate in the abdomen or legs, causing swelling that signals compromised liver function.
The liver also synthesizes most blood clotting factors, including fibrinogen, prothrombin, and factors V, VII, IX, X, XI, and XII. These clotting factors require vitamin K for proper synthesis, which explains why individuals with liver disease may experience bleeding problems or why vitamin K deficiency can lead to coagulation disorders. This protein synthesis function demonstrates why liver disease can affect multiple body systems beyond digestion and detoxification.
Additionally, the liver produces numerous enzymes and transport proteins that carry hormones, vitamins, and minerals throughout your bloodstream. These carrier proteins ensure that essential nutrients reach their target tissues efficiently while maintaining proper concentrations of various substances in your blood.
Liver Immunity and Protection
The liver functions as a crucial component of your body’s immune system, serving as both a filter for bloodborne pathogens and an active participant in immune responses. This immunological role often goes unrecognized, yet it represents one of the liver’s most important protective functions.
Kupffer Cells
Specialized immune cells called Kupffer cells line the liver’s blood vessels, acting as the body’s first line of defense against harmful substances that enter through the digestive system. These cells, which are actually specialized macrophages, constantly scan blood flowing through the liver for bacteria, viruses, damaged cells, and other potentially harmful materials. When they detect threats, Kupffer cells engulf and destroy them, preventing these pathogens from reaching other parts of your body.
This filtering function is particularly important because blood from your intestines flows directly to the liver through the portal vein before circulating to the rest of your body. This arrangement ensures that any bacteria or toxins absorbed from your digestive tract encounter the liver’s immune defenses before they can cause systemic problems.
Filtering Pathogens and Damaged Cells
Beyond Kupffer cells, the liver contains other immune cell populations that help maintain overall health and prevent infections. These cells can recognize and eliminate damaged red blood cells, process cellular debris, and coordinate immune responses when needed. The liver’s immune function also involves producing complement proteins and other immune factors that support your body’s ability to fight infections throughout your system.
The liver’s immune capabilities become particularly evident during infections or inflammatory conditions, when it can increase production of acute-phase proteins that help coordinate your body’s defensive responses. This immune function explains why liver disease can increase susceptibility to infections and why maintaining liver health supports overall immune system function.
Regenerative Capacity: The Liver’s Unique Ability
Among all organs in the human body, the liver possesses an almost miraculous ability to regenerate and repair itself after injury. This remarkable capacity allows the liver to recover from various forms of damage, including toxic exposure, viral infections, and even surgical removal of portions of the organ.
When liver tissue is damaged or removed, the remaining healthy cells can rapidly multiply and restore the organ to its original size and function. This regenerative process is so efficient that the liver can fully regenerate from as little as 25% of its original mass, a capability that has made liver transplantation and surgical resection possible for treating liver cancer and other serious conditions.
The regenerative process involves complex cellular signaling pathways that coordinate cell division, blood vessel formation, and tissue organization. Growth factors and cytokines trigger hepatocytes to exit their normal quiescent state and begin dividing, while other signals ensure that the regenerating tissue maintains proper structure and function. This process typically occurs over several weeks to months, depending on the extent of damage and the individual’s overall health status.
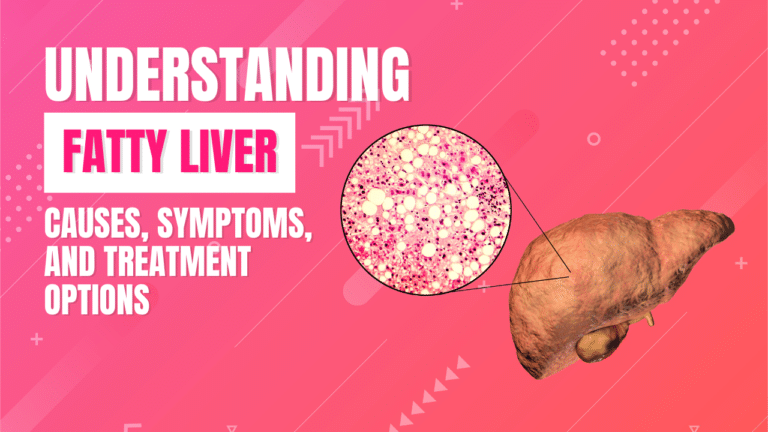
However, this regenerative capacity has limits. Repeated or severe damage can overwhelm the liver’s ability to repair itself, leading to scarring (fibrosis) and eventual cirrhosis. This progression explains why chronic conditions like viral hepatitis, alcohol abuse, or fatty liver disease can eventually cause irreversible liver damage despite the organ’s impressive healing abilities.
Nutrients and Emerging Research
Recent scientific advances have revealed new insights into how specific nutrients support liver function and how cellular energy systems regulate liver metabolism. These discoveries are reshaping our understanding of liver health and opening new avenues for preventing and treating liver disease.
Magnesium plays a critical role in liver energy metabolism and cellular signaling pathways that maintain liver function throughout life. This essential mineral serves as a cofactor for hundreds of enzymatic reactions in the liver, including those involved in protein synthesis, DNA repair, and energy production. Magnesium deficiency can impair liver function and may contribute to the development of fatty liver disease and metabolic dysfunction.
Cutting-edge research has also focused on cellular energy sensors like AMPK (AMP-activated protein kinase), which acts as a master regulator of metabolism in liver cells. AMPK activation influences both glucose and lipid metabolism, helping to maintain metabolic balance and prevent the accumulation of fat in liver cells. Understanding these molecular mechanisms has implications for treating conditions like metabolic dysfunction-associated steatotic liver disease (MASLD) and may lead to new therapeutic approaches for liver-related metabolic disorders.
These emerging research findings highlight the importance of maintaining adequate nutrition and supporting the liver’s natural metabolic processes through lifestyle choices and, when appropriate, targeted supplementation under medical guidance.
Supporting Your Liver’s Health
Maintaining optimal liver health requires a comprehensive approach that combines healthy lifestyle choices with preventive medical care. The liver’s remarkable resilience means that supportive measures can have profound effects on its function and longevity.
A balanced diet rich in antioxidants, fiber, and essential nutrients provides the foundation for liver health. Limiting alcohol consumption, avoiding unnecessary medications, and maintaining a healthy weight help prevent the accumulation of fat in liver cells that can lead to metabolic dysfunction. Regular physical activity supports liver function by improving insulin sensitivity, promoting healthy blood flow, and helping maintain optimal body composition.
Preventive care plays an equally important role in liver health maintenance. Managing underlying conditions like obesity, diabetes, and metabolic syndrome can prevent the development of fatty liver disease and its progression to more serious complications. Vaccination against hepatitis A and B, safe practices to avoid hepatitis C transmission, and regular health screenings help protect against viral liver diseases.
Regular monitoring through comprehensive liver function testing can detect early signs of liver dysfunction before symptoms develop. Walk-In Lab’s Liver Function Panel provides convenient access to essential tests including ALT, AST, bilirubin, and albumin levels, offering valuable insights into liver health status. Additional testing for nutrients like magnesium and comprehensive metabolic panels can provide a complete picture of factors affecting liver function.
Early detection of liver problems allows for timely intervention and lifestyle modifications that can prevent progression to more serious conditions. Regular testing is particularly important for individuals with risk factors such as family history of liver disease, metabolic syndrome, or previous exposure to hepatotoxic substances.
Frequently Asked Questions
What is the liver’s main function?
The liver serves multiple critical functions, but its primary role is as the body’s detoxification center and metabolic hub. It processes nutrients from food, neutralizes harmful substances like toxins and medications, produces bile for digestion, synthesizes essential proteins, and regulates blood sugar levels. Think of the liver as your body’s chemical processing plant, working continuously to maintain the proper balance of substances in your bloodstream.
How does the liver detoxify substances?
The liver detoxifies substances through a sophisticated two-phase process. Phase I uses cytochrome P450 enzymes to chemically modify toxins through oxidation, reduction, or hydrolysis. Phase II involves conjugation reactions where the liver attaches water-soluble molecules to these modified toxins, making them easier to eliminate through bile or urine. This system can process thousands of different compounds, from alcohol and medications to environmental pollutants and metabolic waste products.
Why is bile important?
Bile serves two essential functions: facilitating fat digestion and eliminating waste products. The bile salts in bile act like biological detergents, breaking down large fat molecules into smaller droplets that digestive enzymes can process more effectively. Bile also serves as the primary route for eliminating certain waste products, particularly bilirubin from old red blood cell breakdown. When bile production or flow is impaired, it can lead to digestive problems and the accumulation of waste products in the blood.
Can the liver regenerate if damaged?
Yes, the liver has remarkable regenerative capacity and can restore itself to full size and function from as little as 25% of its original mass. When liver tissue is damaged, the remaining healthy cells rapidly multiply and reorganize to replace lost tissue. This process typically takes weeks to months and involves complex cellular signaling that coordinates cell division and tissue restructuring. However, repeated or severe damage can overwhelm this regenerative capacity, leading to scarring and permanent dysfunction.
What roles do immune cells play in the liver?
The liver contains specialized immune cells, particularly Kupffer cells, that serve as the body’s first line of defense against bloodborne pathogens and toxins. These cells constantly filter blood flowing through the liver, removing bacteria, viruses, damaged cells, and other harmful materials before they can reach other organs. The liver also produces immune proteins and coordinates inflammatory responses, making it a crucial component of the body’s overall immune system.
Conclusion
Your liver truly deserves recognition as the body’s master detoxifier and metabolic powerhouse. This remarkable organ simultaneously processes nutrients, neutralizes toxins, produces essential proteins, supports digestion through bile production, and protects against infections through its immune functions. The liver’s unique regenerative capacity further demonstrates its crucial role in maintaining your health and vitality.
Understanding how your liver works empowers you to make informed decisions about your health and recognize the importance of preventive care. Regular monitoring through comprehensive liver function testing, combined with healthy lifestyle choices, provides the foundation for maintaining optimal liver health throughout your life. The liver’s resilience means that supportive measures can have profound positive effects, while early detection of problems allows for timely interventions that can prevent serious complications.
Take charge of your liver health today by ordering a comprehensive Liver Function Panel through Walk-In Lab. With convenient, confidential testing and direct access to results, you can gain valuable insights into your liver’s current status and take proactive steps to support this vital organ’s continued function.
This article is for informational purposes only and is not intended as medical advice. Always consult with healthcare professionals for personalized medical guidance and before making decisions about your health.